Mason (2013) stated that, “shame safeguards the spirit.” When shame is our reality, we don’t feel good about ourselves. Shame is generally learned from experiences in our most vulnerable developmental years. However, since memories can be moved/restored through the process of memory reconsolidation (Ecker, Ticic, & Hulley, 2012), our reality is subjective to the meaning we give it. This teaching may question our foundation of what composes our reality. Even more to the point, it calls into question the very essence of who we are.
In the Institute for Creative Mindfulness EMDR therapy training, we explore the client’s trauma targets using a thematic approach. Addressing traumas in a thematic way allows the client to address what they believe and how they feel about themselves in order to rewrite, renew, or own their story. Because of this, anything can be targeted with EMDR, if it holds adaptive or maladaptive value and the client can emotionally access it. However, what about the experiences that are there but not recognized consciously or that started before narrative or declarative memory developed in the brain?
Let me first acknowledge the difference between what I am presenting and Paulsen and O’Shea’s (2017) “When There Are No Words” protocol. Paulsen and O’Shea’s stance is that their protocol “reset the hardwired neuro-affect circuits” and this is done in Phase 2 Preparation. What I am presenting here is an option for clinicians who are not trained to do “When There Are No Words” (or are having difficulty following the nuances of protocol they downloaded off the web). Paulsen and O’Shea’s protocol can be helpful for clients; however, I also believe that accessing implicit memories through what I am suggesting holds additional value on two levels. One, it is a good and safer place to get “buy-in” from a client, and two, if it does not go as we would hope, it can be “diagnostic.” I want to gain access to my client’s earliest wounds. What I am proposing is more of a “Phase 2.5” intervention that links Phase 2 and the reprocessing Phases 3-6 (Marich, 2019). This intervention allows clinicians to address our client’s preverbal schemas with any and all thematically shame-based core belief clusters because this is actually where the cluster begins.
Shape and Color Set-up: While taking clients trauma history (Phase 1) and assessing core beliefs (Phase 3), I am looking to put their core beliefs in two categories: shame-based (i.e., I am bad, I am worthless) and fear-based (i.e., I am in danger, I am powerless) core beliefs. Before floating back on a core belief I will ask, “Do any of these shame-based beliefs just feel like they have always been there?” (I will either ask this during Phase 1, Client History or Phase 3 Assessment.) Nine times out of ten, clients will identify a shame-based negative cognition. If the clients pick a fear-based cognition like “I am in danger,” I stay away from it because it is most likely linked directly to an event that can be directly recalled and I am not trying to have them start reprocessing a direct memory. If this happens, I will guide them towards a shame-based core belief.
After resourcing in Preparation (Phase 2), assessing targets (Phase 3), and establishing some kind of stop signal, I then have the client create a target of the core belief felt-sense by asking, “What shape and color would represent this ‘has always been there’ belief?” Once the client has the image (and negative cognition) then it is standard protocol time (i.e., Phases 4-7 and Phase 8 in the next session). Future template can be done but I feel that because I am priming the pump and that there are declarative memories still to go, I wait until I see how the client responses to the process and do future templates with memories that are able to be recalled.
Rationale: I am trying to see what is going on under the hood and also preparing their memory system for reprocessing shifts. My reference to the shape and color or image comes from Mark Grant’s work on pain management (1995). Paulsen and O’Shea also use this strategy; they do not, however, want you to activate the client. My position is that if we are addressing the client’s schema, that they are feeling all the time, they are already activated. Again, I suggest doing this on shame-based themes and not fear-based ones because I believe it is safer and the client is less likely to activate actual memories. However, activating shame-based memories does happen. In this case, I will guide them back to target or go back to resourcing. If the client has too much shame then the standard practices of creating some distance between the client and image, having the client pendulate, or taking only doing a fragment is advised. To further support my position, if the theme carries a high SUDs, which it normally does, Shapiro (2018) suggests doing a more intense early memory first because if they can do this, then they can handle whatever else is to come. Lastly, and for obvious reasons, this is actually the start of the cluster.
Buy In: Starting with a shape and a color allows the client to test-drive reprocessing. When clients open up to reprocessing they are opening themselves to their own healing. When that positive shift happens, they have experienced something that is effective and they will have more buy-in into their treatment. When, as the clinician, we express that it is a more indirect way of reprocessing EMDR, it implies that we are starting someplace safer. Clients appreciate this. Also, since their core beliefs are something that they already feel and live with on a daily basis they are familiar with it and okay talking about this more than their traumas. Once they have seen a shift in this, then now know and have direct experience that EMDR therapy works for them.
Diagnostic: Doing this is also a good test run to see if the person is able to do the deeper work and can be diagnostic in the sense that you get a feel for the clients protective/dissociative system and their level of preparedness on an unconscious level. Ideally, this is assessed in Phases 1-3 of EMDR but it is not always apparent on an unconscious level. Obviously, we need to have rapport, do assessments like the DES (at a bare minimum), and use our clinical judgment but it is not always obvious how someone’s unconscious will respond. If the client picks a shape and a color that goes from dark to something light and has freed something in them or they feel lighter, then chances are they are ready to do the deeper work that they are coming to us for. Additionally, they now have direct experience with feeling a shift in their emotional body, particularly with something that feels like it has always been there, again, we get a lot of buy-in.
As clinicians, we also get a lot of information regarding diagnostics if the client cannot remember their early childhood and/or by seeing if the client can do calm/safe place or container. If they cannot do this effectively then there is more going on in their dissociative process that is worth discussing with them (Paulsen, 2009). I started doing the Color and Shape Set-up before having the Dissociative Table (Paulsen, 2009) as a tool in my EMDR toolbox. I now will start with the dissociative table, O’Shea and Paulsen’s “When There Are No Words,” and then this Color and Shape Set-up, when appropriate.
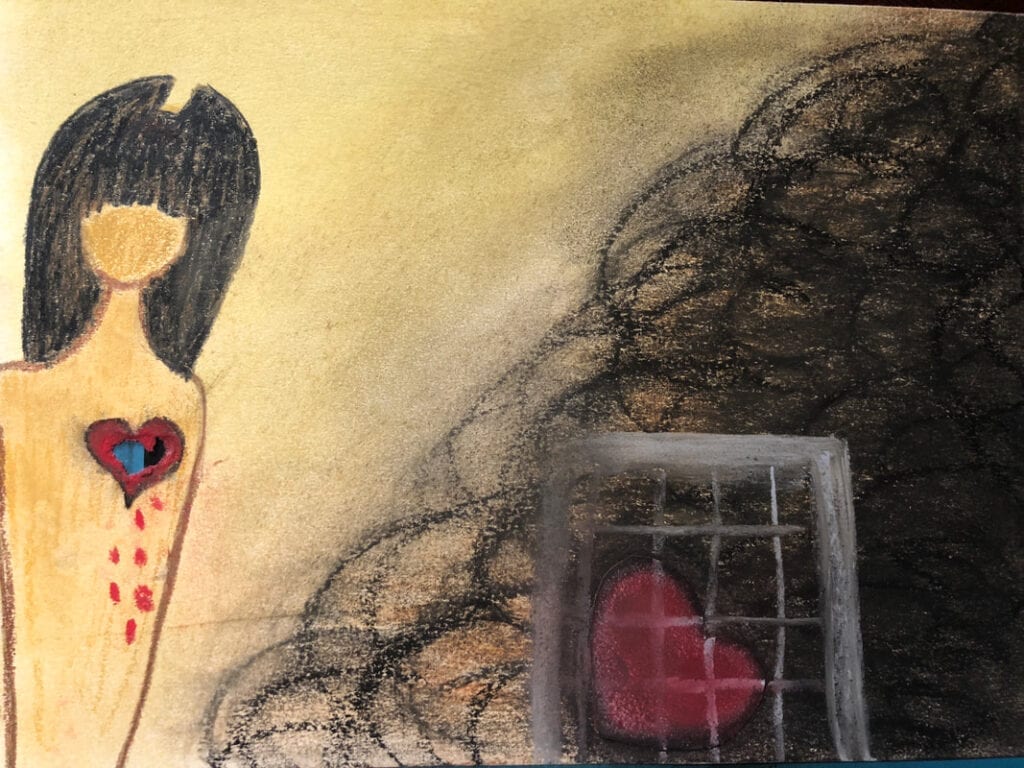
Observations: The shame color/shape/image is usually dark. When reprocessing goes well, people get to a bright and lively color and/or translucent image. Sometimes, it just disappears. When it does not go “right” the image usually stays the same and clients will say, “it does not feel like it is going to move.” This is clinically telling and potentially diagnostic so more psycho-education and resourcing may be needed. Yes, some clients will have the wherewithal to identify that “it has always been there” or “I just feel it.” This insight may indicate where they are at in their readiness to do deeper reprocessing. This suggests to me that they are highly attuned to their body and are already primed to do EMDR or trauma reprocessing.
Generalization: Generalization is when the client starts to reprocess all of the thematic memories in a cluster (Ecker, Ticic, & Hulley, 2012). This happens because once a core belief is resolved in an earlier memory the lesson learned is applied to other similar situations. Since the brain works through making associations, any association can connect to the neuro-network that rides this theme is going to be impacted, hence has the opportunity to be reprocessed. If the client is consciously and unconsciously open to healing then they are going to do a great deal of work starting in this way.
Populations: I particularly love doing this with people are addressing their addictions because they are usually living in their right-brain processes. This also goes for people who are creative and children between the ages of 2-12 respectfully. Highly motivated adolescents respond well but other adolescents find it weird. Similarly, I like doing this with personality disorders as well because it gives them the opportunity to allow shifts to happen, and/or challenges them if it does not. It provides experiential material to work on. For more left-brained people, it can be a challenge but it gives them the opportunity to connect to their more emotional side.
Healing Light: Also, consider that this can be done in combination with healing light. I will have clients get their SUDS down to a like 2-3 and then I will perform the healing light or Light Stream on the remainder. I have witnessed some very spiritual and religious experiences by doing this.
Target Order: When I do a floatback and get the earliest memory if it is not between the ages of 2-5, I have my client’s try and float further back. Because of what I am purposing, with regard to schemas and shame-based beliefs, it is implied that the earliest recall memories are going to be represented around the chronological ages of 2 to 5. Our expertise that tells us that the schemas started before the age of 2.
Clients are coming to us for our expertise on the therapeutic process and trauma etiology, which can conflict with letting the client lead or decide what memory to do first. If I have a client who wants to address something more recent or only one specific memory then I will have them try the Color and Shape Set-up first as a test run. Similarly, if there is no discrete memory (Greenwald, 2007) or test run memory to do, I also do this. There are times when having the client lead or pick a memory that they want to work on can be effective. Allowing the client to lead the selection of targets without any guidance, however, can be what creates more work later. So, we have to have a good case conceptualization in order to maximize the outcomes of healing and our conceptualization has to be based on trauma-informed care, which means to me, safety first. What this writing ultimately comes down to is that traumas are compounded in the memory network because our neuro-networks are associative and by previous traumas so starting off at the earliest is the safest and will be more likely going to produce better outcomes (Greenwald, 2007).
Feel free to contact me for individual consultation or attend my weekly group on Friday’s 12-2pm EST.
References
Ecker, B., Ticic, R., & Hulley, L. (2012). Unlocking the emotional brain: Eliminating symptoms at their roots using memory reconsolidation. New York, NY: Routledge.
Grant, M. (1995). From https://emdrtherapyvolusia.com/wp-content/uploads/2016/12/Mark_Grants_Pain_Protocol.pdf Retrieved on 2/8/19
Greenwald, R. (2007). EMDR: Within a phase model of trauma-informed treatment. Binghamton, NY: Haworth Press, Inc.
Marich, J. (2019). EMDR Therapy Phase 2.5: Honoring a Wider Context for Cnhanced Preparation. [Blog Post] Retrieved from https://www.instituteforcreativemindfulness.com/icm-blog-redefine-therapy/emdr-therapy-phase-25-honoring-a-wider-context-for-enhanced-preparation-by-jamie-marich-phd-lpcc-s-licdc-cs-reat-ryt-200
Mason, M. (2013). Women and shame: Kin and Culture. In. Claudia Bepko (Ed.), Feminism and addiction (pp. 175-194). New York, NY: Routledge
Paulsen, S. (2009). Looking through the eyes of trauma and dissociation: An illustrated guide for EMDR therapists and clients. Bainbridge Island, WA: A Bainbridge Institute for Integrative Psychology Publication.
Paulsen, S., & O’Shea, K. (2017). When there are no words: Repairing early trauma and neglect from the attachment period with EMDR Therapy. Bainbridge Island, WA: A Bainbridge Institute for Integrative Psychology Publication.
Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols, and procedures (3rd ed). New York, NY: Guilford Press.




2 Responses
This seems like a really good idea. I have a 19 year old client whose touchstone is sexual abuse as a child by some other neighborhood children. We have already worked a bit with externalizing the shame on paper so I feel like this would be a great test run.
I have a question. Does the client pair the negative cognition with the personification of the shame during the extinction phase and then also observe what happens to the shape when doing installing the new belief?